You can’t avoid seeing all the hearts displayed this month for Valentine’s Day. I feel like the stores started stocking heart-shaped candies right after they put away the noisemakers for New Year’s celebrations. Besides seeking out your one true love this month, February is also American Heart Month. Usually, the campaigns for American Heart Month feature celebrities in beautiful red gowns, reminding us to take heart health seriously. Those advertisements are correct; prioritizing cardiovascular health is of the utmost importance, and incorporating healthy habits into daily life can help decrease the risk of developing heart disease. Heart disease remains the leading cause of death for Americans, and prevention is always preferable. One’s propensity to develop heart disease is a mix of genetics, lifestyle, and social factors, so there are ways to lessen your risk of heart disease by making positive changes.
Since heart disease is a catch-all term for diseases that affect the structure and function of the heart, I’m going to focus on two specific conditions, acute coronary syndrome (AKA a heart attack) and heart failure, and how hospitals can vary in their ability to treat patients.
Acute coronary syndrome: Can your hospital get it all done in time?
I didn’t get to see the episode of And Just Like That, where Mr. Big dies from a heart attack. But if it is anything like other television depictions of acute coronary syndrome (ACS), it probably went something like this: Mr. Big has chest pain….Mr. Big is dead. Though sudden death is a possibility, it isn’t the guaranteed outcome for people experiencing acute coronary syndrome. Also, not everyone gets the chest pain/pressure symptoms that are classically thought of as the harbingers of a heart attack. People can experience the symptoms of ACS differently, depending on their age, sex, and other medical conditions. For example, many women experience ACS symptoms such as shortness of breath, dizziness, back pain, or headache. Check out this video from the American Heart Association of a funny yet accurate depiction of ACS symptoms in women.
To adequately diagnose and treat ACS, time is of the essence. How fast a patient gets to the hospital for an ECG, lab work, and assessment by a cardiologist for possible intervention can make a massive difference in a patient’s outcome. So, the American College of Cardiology has outlined a timeline for diagnosing and treating chest pain (fig 1) that hospitals should strive to achieve. The goal is to assess and treat patients within the “golden hour” (one hour after symptoms of ACS start) and get them ready for treatment in a cath lab within 30 minutes of coming to the hospital when appropriate.
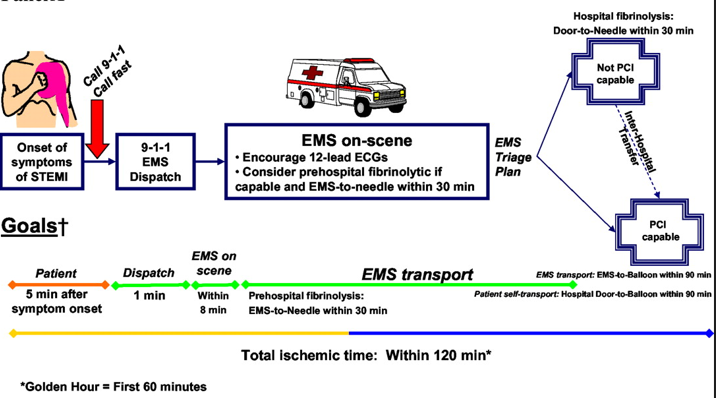
Fig 1: Time Line to Diagnose and Treat ACS.
Credit- ACC/AHA Guidelines for the Management of Patients With ST-Elevation Myocardial Infarction—Executive Summary
Circulation. 2004;110:588–636
Does Your Hospital Have a Cath Lab?
How well a hospital can treat ACS depends on the clinicians and equipment available, specifically a cardiac cath lab. A cardiac cath lab is a specialized procedure room where interventional cardiologists do procedures to diagnose and treat ACS by placing stents in the heart’s blood vessels. For a hospital to meet the time guidelines discussed above, it must be able to mobilize the cath lab team quickly. An interventional cardiologist must be available to diagnose and treat patients at all hours.
Does your local hospital have a cath lab? There are 6120 hospitals in the United States and only 1700 cath labs. You should research whether there is a cath lab at your closest hospital or somewhere else nearby so you know where to go if you or a loved one has symptoms concerning for a heart attack. You can maximize that “golden hour” by going directly to the hospital that has a cath lab available, should you need it.
A cath lab isn’t just for treating ACS. Interventional cardiologists can also treat conditions such as arrhythmias in the cath lab. Non-interventional cardiologists also rely on the cath lab to help them diagnose and treat patients; for example, a patient can be sent to the cath lab for the interventionalist to take detailed measurements of the patient’s heart function, allowing the cardiologist to optimize the medications needed to treat heart failure.
Heart Failure: Who is on your team?
Heart failure is a condition defined by a decrease in the effectiveness of the heart’s ability to pump blood that causes symptoms such as weakness, shortness of breath, and the build-up of excess fluid. Though there are lots of reasons a person can develop heart failure, treatment generally focuses on improving the heart’s ability to pump blood by decreasing the amount of work the heart has to do. This is accomplished by removing excess fluid, decreasing blood pressure, and improving the efficiency of heartbeats.
Unlike ACS, the treatment of heart failure doesn’t generally require a procedure; instead, physicians rely on various medications to achieve the desired effects. But this doesn’t mean specialized treatments and specialists aren’t a boon to patients. Understanding how to treat heart failure is considered a cornerstone of hospital-based care, and most hospitalists will tell you they’re comfortable treating patients with heart failure. Yet, there are ways hospitals can work to improve the care of heart failure patients.
Using clinical guidelines to create specialized “care tracks” or “order sets” is one option hospitals can try to improve heart failure outcomes. Employing specialized clinicians who focus solely on treating and preventing heart failure while working closely with patients after discharge is another way a hospital may improve its care of heart failure patients. Some hospitals have created separate teams to treat heart failure patients so that every physician, nurse, and other clinical provider is laser-focused on heart failure. Using a multidisciplinary team to treat heart failure is known to improve patient outcomes and is recommended by the American College of Cardiology and the American Heart Association.
Another way hospitals may seek to improve outcomes for heart failure patients is to bolster care and education after discharge from the hospital. Working closely with outpatient cardiologists and primary care doctors to give extra patient education and support after discharge can decrease the chances of readmission. Insurance agencies may incentivize hospitals and outpatient providers to work together so patients can access office appointments and/or telehealth follow-ups relatively soon after discharge.
The Cardiologist’s Office and the Hosptial: A Relationship to Cherish.
After being treated in the hospital for ACS or heart failure, you are likely going to need several follow-up appointments with your cardiologist. If your outpatient cardiologist works closely with the hospital that cared for you, this can improve outcomes and experience. Creating a sustainable care plan for heart disease hinges on the ability of providers to share information and tap into resources for patients seamlessly. In cases where the hospital and your outpatient providers are not closely tied, be sure to ask for records to be sent directly to the cardiologist and primary care provider’s offices before your first appointments.
TLDR
Preventing, diagnosing, and treating heart disease requires input from a multidisciplinary team of healthcare providers. Those providers need to be supported by a hospital with the infrastructure to respond thoughtfully and quickly and to coordinate care well after discharge. Take some time to learn what initiatives the hospitals in your area have to support patients with heart failure and if there is a cath lab close by that can treat ACS.
As a hospitalist, I will spend the last few days of February working in a hospital, with halls still covered by a few stray Valentine’s Day decorations. As much as I can try to romanticize my days at work, I don’t recommend going to the hospital for a romantic getaway. But your local hospital could help with other matters of the heart.
For more information on what to look for in hospital-based care, order a copy of Prescription for Admission, a Doctor’s Guide for Navigating the Hospital, Advocating for Yourself, and Having a Better Hospitalization.